How to Address a Denied Claim in MedBatch
If a claim has been denied, the error code will provide information regarding the denial reason. Depending on the denial reason, the claim can be edited and resubmitted, or you can reach out to eMedNY for more information at 1-800-343-9000.
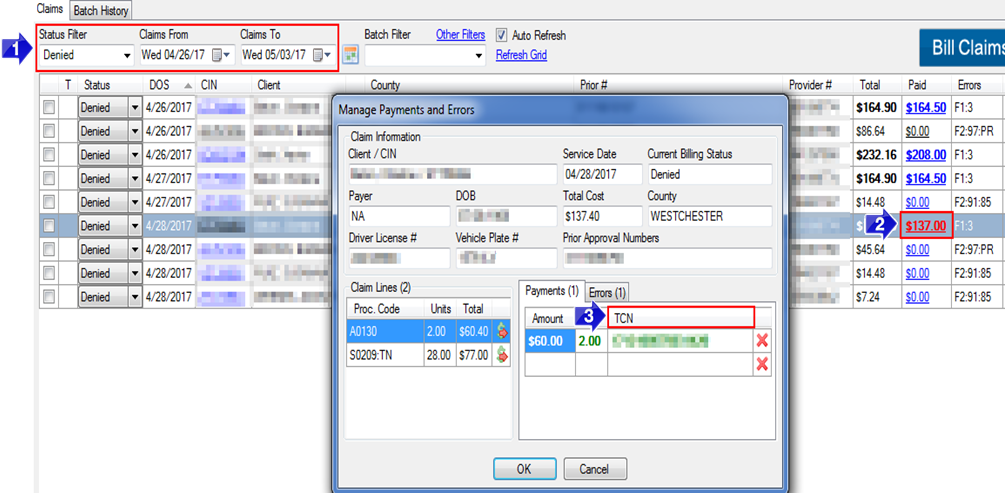
1. To view Denied claims, set the Status Filter to Denied and enter the Claims From and Claims To dates for the claims you would like to view within the grid.
2. To view more information about a denied claim, click on the dollar amount in the Paid The Manage Payments and Errors window will open.
3. The TCN can be found in this window. When reaching out to eMedNY regarding a denied claim, you will need to provide the TCN.
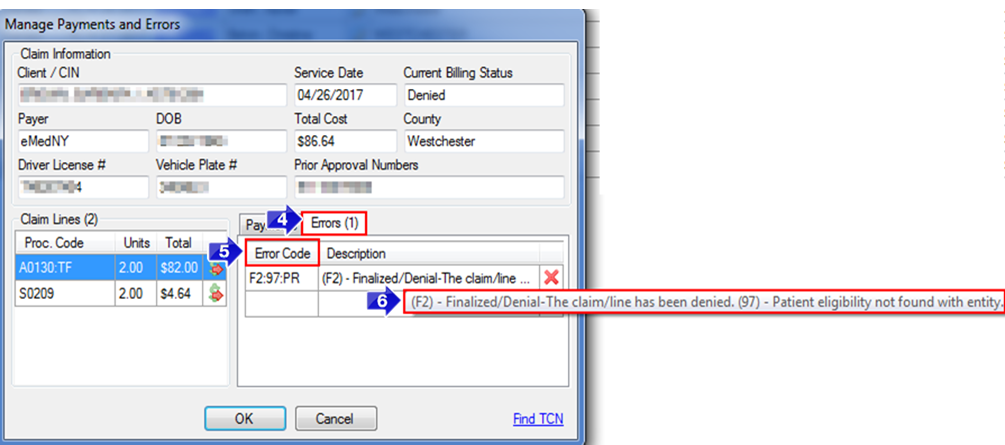
4. The Errors tab will provide the Error Code and a Description of the error.
5. The Error Code column will display any error codes that the claim has received.
6. Hover over the Description to view the full description of the Error Code.
Depending on the Error Code, you may be able to edit and resubmit the claim. If the Description of the Error Code does not provide enough information, you can call eMedNY at 1-800-343-9000 and provide the TCN as a reference for that claim.
![New Founders Software-White.png]](https://help.intelligentbits.com/hs-fs/hubfs/New%20Founders%20Software-White.png?height=50&name=New%20Founders%20Software-White.png)