How to Enter a Delay Reason Code in MedBatch
Medicaid claims that are more than 90 days old typically require a Delay Reason Code.
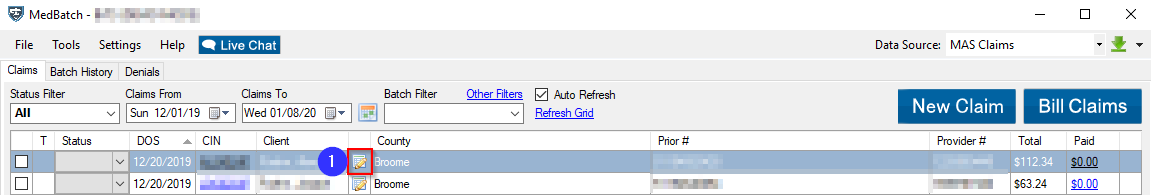
1. To enter this code on a claim, click the Edit Claim icon to open the Edit Claim window.
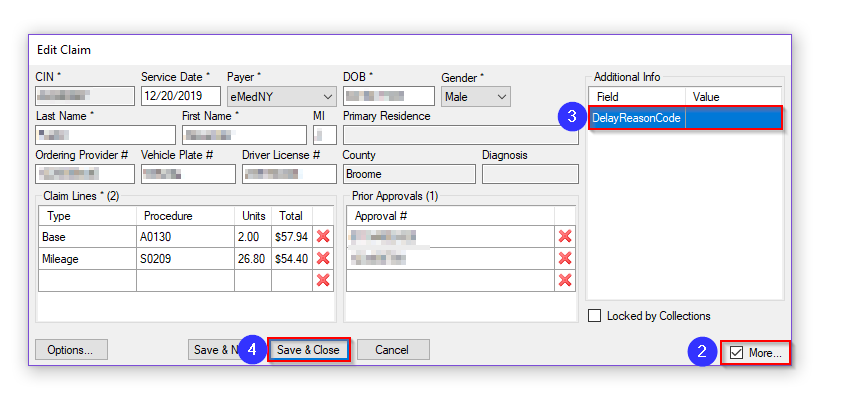
2. In the lower right corner, check the box labeled More. Clicking this will open the Additional Info tab.
3. Type the Delay Reason Code into the Value field.
4. Click Save. The claim is now ready to bill.
Follow this link for a list of Delay Reason Codes in NYS:
https://www.emedny.org/HIPAA/QuickRefDocs/FOD-7001_Sub_Claims_Over_90_days_Old.pdf
Related Articles:
How to Bill My Claims
How to Rebill a Claim
How Do I Edit Claims?
Key Terms:
Claims, Delay Reason Code, Edit Claim
![New Founders Software-White.png]](https://help.intelligentbits.com/hs-fs/hubfs/New%20Founders%20Software-White.png?height=50&name=New%20Founders%20Software-White.png)